
Patellofemoral Pain Syndrome is a challenging knee injury because even in 2021 the exact causes remain unclear and no single treatment works equally well for everyone.
Newer research examined different treatment approaches for different subgroups among those with patellofemoral pain syndrome and while the results are promising, we’re still far from a complete understanding of the injury.
This page will show you how to best get rid of patellofemoral pain syndrome, based on what we know today.
Symptoms
The symptoms of patellofemoral pain syndrome are1:
- Diffuse pain behind or around the kneecap
- Squatting, climbing stairs, running, sitting, jumping, or kneeling usually worsen the symptoms
Usually the pain in PFPS increases gradually2 and it often becomes chronic3. Participants of the research studies on patellofemoral pain syndrome had symptom durations as high as 3+ years4.

Patellofemoral pain syndrome can also lead to psychological symptoms such as kinesiophobia5 (fear of pain due to movement), elevated anxiety, depression, and pain catastrophizing6 (assuming the worst will happen).
Diagnosis
Unfortunately, there is no gold standard diagnostic test to confirm the diagnosis of patellofemoral pain syndrome7. Your doctor will diagnose the injury through a physical examination and by inquiring about your pain history8.

Your doctor will then have to rule out knee injuries with similar symptoms through differential diagnosis9. Injuries that could mimic the pain of PFPS are10:
- Hoffa’s syndrome
- Osgood Schlatter Syndrome
- Sindig-Larsen Syndrome
- IT Band Syndrome
- Patellar Tendonitis
- Plica syndrome
- Intra-articular injuries such as osteoarthritis or rheumatoid arthritis
- Traumatic injuries like patellar fractures, injured ligaments, and meniscal tears
Imaging tests such as MRI or ultrasound can be useful for a diagnosis via exclusion, but they can’t help diagnose patellofemoral pain syndrome directly11.
Causes and Risk Factors
Patellofemoral Pain Syndrome can occur in athletes and non-athletes12. Its exact causes remain unclear13, even to this day, which is why it is also described as a “black hole” in orthopedic medicine14. Yet, we do have a list of potential causes15:
- Patellar maltracking16
- Muscle weakness (e.g., quads17, hip abductors and external rotators18, trunk side flexors19)
- Delayed vastus medialis muscle activation, strength, or morphology20
- Lack of flexibility of leg muscles (e.g., calves, hamstrings, and quads21)
- Overpronation22
- Prolonged and excessive forces pulling on the patella in lateral direction23
- Abnormal femoral24, tibial25, or foot rotation26
- Excessive hip adduction27 during movement
- Misalignment of the hip during movement28 (e.g., contralateral pelvic drop)
- Reduced strength and or motor control of the trunk and core muscles29
- Anatomical factors30 (e.g., patella alta, hypoplasia of medial patellar facet, shallow trochlear groove31, femoral anteversion and inclination32)
- Overloaded medial stabilization structures (retinaculum) in the knee due to excessive lateral forces33
- Faulty running technique34
- Female gender35
- Reduced blood flow in or around the kneecap36
- Reduced proprioception37
- Reduced extension ability of the big toe38
To a large extent it remains unclear which of these factors are causative and which are the result of activity reduction due to pain39.

Additionally, causes of patellofemoral pain syndrome are likely different between genders40 and even in one gender, different subgroups of PFPS likely exist41.
Treatment
Treating patellofemoral pain syndrome successfully is challenging, because 10 people with PFPS may well have 10 different causes that contribute to their pain42. However, based on the research I’ve read, I would suggest the following treatment steps, ideally in that order.
Step 1) Work on the Mental Side
One study found that participants with patellofemoral pain syndrome looked for social support less than the healthy control group43. The same research also revealed that those with PFPS were less able to relax when faced with a problem.
Other research revealed that misconceptions about the pain caused by the injury correlate with lower function and, ironically, higher pain44.

You can soften the negative psychological effect the injury can have by reminding yourself that:
-
While PFPS is complex and frustrating, imaging scans of the knee will often come back clean. This means that in many cases, the structures inside the knee are healthy.
In other words, chances are you will get significantly better just by doing a couple of exercises.
-
Physical and psychological stress can both contribute to the pain45. This means your recovery will go better if you relax. Don’t obsess over your training, over “lost” progress, or even about the pain.
Putting yourself under pressure because you got hurt will slow your recovery. It is what is for now and with the right approach it will get better. Give your body the time it needs.
- Chances are you will notice a significant improvement within a month of doing the right exercises for your individual situation46. Don’t expect progress to happen in just a few weeks or even days. It takes a while.
- Resting the knee is important to aid your recovery, but ignoring the injury and leaving it unaddressed will lead to more pain and frustration in the future.
Now is the best time to work on it.
Yes, we’re still a fair bit away from a complete understanding of patellofemoral pain syndrome, but the treatments we’ve developed so far do work in most cases.
Step 2) Improve Strength & Flexibility
The treatment exercises for patellofemoral pain syndrome should always be done without pain or in the pain-free range of motion.
The following list summarizes what you need to work on and provides some example exercises.
A) Improve the strength of:
- Hip abductors (exercise: side-lying hip abductions)
- Hip external rotators (exercise: side-lying clamshells)
- Hip extension (exercise: two- and single-legged glute bridges)
- Calves (exercise: calf raises)
- Quadriceps Muscles (exercises: wall sit, leg press, leg extension – depending on what’s tolerated)
- Hamstrings (exercises: deadlifts, single-leg deadlifts)
- Trunk Side Flexors (exercises: side bridge)
- Hip Hike Exercise
You can adapt the exercises based on how your knee reacts:
If there is pain during knee extension, open kinetic chain exercises with more knee flexion (40 – 90° knee angle) may work better.
If deeper knee flexion is painful, working with closed kinetic chain exercises in lower knee flexion (0 – 40° knee angle) may produce better results47.

As you can see, it is not enough to just work on the muscles of the knee. In fact, combining knee with hip exercises delivered superior results in research48.
B) Massage, stretch, and mobilize:
- Calves
- Quads
- Hamstrings
- Hip Flexors
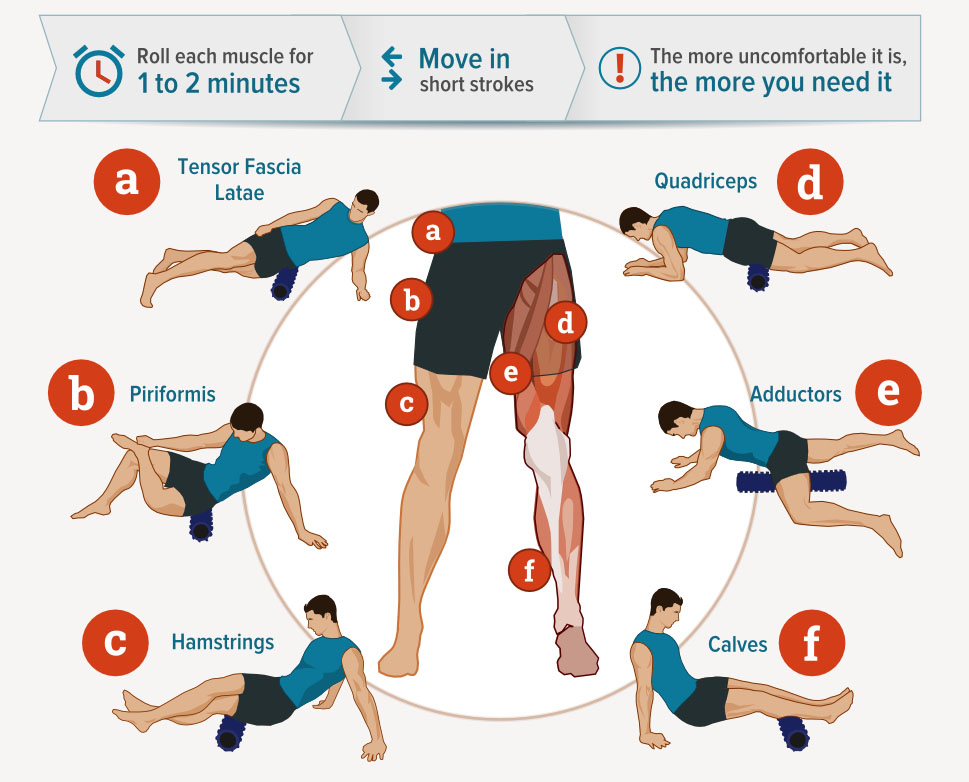
The standard foam-rolling sequence works well in addition to whatever stretches you like to do for the respective muscles. Here’s a stretching video that provides some exercise ideas:
Step 3) Improve Motor Control
Muscle strengthening alone is not enough to change the way someone moves49, so we also need to work on motor control directly.
Interestingly, one study on dancers found that the injury was less common among those with LOWER range of motion at the foot, ankle, and hip50. This suggests that improving stability (i.e., ability to prevent unwanted movement) may be beneficial for some of those with PFPS.
Exercises I would suggest are:
A) Balance Drill

Stand with your feet hip-width apart and pointed forward.
Imagine your knees are flashlights and point their beams straight ahead.
Now balance on one foot while making sure the knee of that leg keeps pointing straight forward. Do not let it point towards the other side.
Keep your hips and shoulders parallel to the ground as you lift the foot.
Don’t lean to one side and don’t lift one side’s hip up.
The movement should happen almost completely in the legs. Do not move the upper body.
B) Core Activation Work
This topic cannot be covered in just a few paragraphs, but here’s a simple exercise to get you started:
Lie on your back with your knees flexed and feet on the ground.
Make sure your lower back touches the ground.
Keep the lower back in touch with the ground and then begin to walk your feet out until your legs are straight or until your lower back begins to lift.
Brace your core muscles so that your lower back stays on the ground throughout the exercise. You should feel it partly in your abs, but also in the muscles on the side of your abs.

Once you can control your hip movement you can begin doing leg raises with bent knees to make it more challenging.
C) Step-Ups & Step-Downs
Once you can control the position of your hip and torso in the balance drill you can try step-ups.
Stand in front of a 10-inch box or step with your feet hip-width apart and pointed forward.
Place one foot on the box so that it points straight ahead.

Step up slowly, without momentum, while pointing your knee straight ahead.
Keep your hips and shoulders parallel to the ground, just like in the balance drill.
Summary
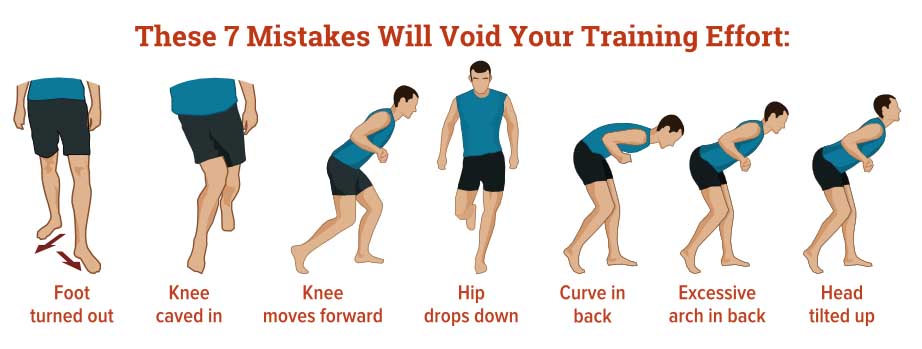
These are very basic motor control drills to help you get started. The details required by a full program would be too much too cover here. However, the technique cornerstones are the same for all standing exercises:
- Feet hip-width apart, parallel, and pointed straight forward (not turned out to the side)
- Knees pointed straight ahead and aligned over the toes (not moved towards the mid-line of the body – keep the knees apart)
- Hips and shoulders remain parallel to the ground (don’t lean sideways to compensate for weak hips)
Stick to those rules in all movements you do throughout your day.
Step 4) Use Adjunct Treatments If Necessary
Certain adjunct treatments have worked well for some people with patellofemoral pain syndrome. These include:
- Icing for short-term pain management51
- Taping (benefit should be felt almost immediately, if not it likely won’t help you)
- Orthotics (beneficial for people with over-pronation/flat feet)
- Chiropractic adjustments (expert consensus is against back manipulation for PFPS52, but some low-quality studies showed benefits53)
- Dry Needling & Acupuncture54
These additional treatments can be beneficial, but they do not replace the need for strengthening exercises and for improving motor control as mentioned earlier.
Step 5) Work on Gait & Running Technique
Research on gait retraining for patellofemoral pain syndrome has repeatedly produced good results55. You can practice this by walking on a treadmill in front of a mirror or by recording yourself.
The technique cues are the same as for the motor control exercises we talked about earlier (feet forward, knees forward and part, hip and shoulders parallel to the ground).

Studies on running technique showed that running with a higher cadence, shorter stride length, and – most importantly – with a forefoot strike led to reduced symptoms in those with patellofemoral pain syndrome.
So once you return to running, focus on landing on the balls of your feet and taking shorter steps. Be aware that calf soreness can occur as a side-effect56, so increase mileage gradually.
Your Rehab Plan
This page is just a very good starting point for rehab of patellofemoral pain syndrome. It is not meant to be exhaustive.
You can use my suggestions as scaffolding, around which you can then construct your own rehab plan, depending on your body’s needs and your doctor’s advice.
I hope you can get well soon.
– Martin
Footnotes
2 Jensen et al. 1999, p. 522
3 Witvrouw et al. 2000, p. 480; IRELAND et al. 2003, p. 671; Rathleff et al. 2013, p. 5
4 Callaghan, Oldham 2004, p. 959; Robinson, Nee 2007, p. 236; Sutlive et al. 2004, p. 54; Fukuda et al. 2012, p. 826; Baldon, Rodrigo de Marche et al. 2015, p. 1485; Collins et al. 2009, p. 163
5 Priore et al. 2020, p. 613
6 Selhorst et al. 2021, p. 1268
7 Cook et al. 2010, p. 18; van der Heijden, Rianne A et al. 2015, p. 13; Fernandez Cuadros, Marcos Edgar et al. 2017, p. 204
8 Cook et al. 2010, p. 22
9 Rees et al. 2019, p. 227
10 van der Heijden, Rianne A et al. 2015, p. 9; van Cant et al. 2017, p. 299
11 Haim et al. 2006, p. 227
12 Earl, Hoch 2011, p. 154
13 Leibbrandt, Louw 2018, p. 218; van Linschoten et al. 2009, p. 1; van der Heijden, Rianne A et al. 2016, p. 111; Fernandez Cuadros, Marcos Edgar et al. 2017, p. 203; Rees et al. 2019, p. 227; Matthews et al. 2020, p. 1416; van der Heijden, Rianne A et al. 2015, p. 13
14 Yañez-Álvarez et al. 2020, p. 839
15 Saltychev et al. 2018, p. 393
16 Draper et al. 2009, p. 572; Lankhorst et al. 2013, p. 197; DUFFEY et al. 2000, p. 1830
17 Neal et al. 2019, p. 273
18 Willson, Davis 2009, p. 81; Dierks et al. 2008, p. 452; IRELAND et al. 2003, p. 673; Ferber et al. 2011, p. 145; Magalhães et al. 2010; Lankhorst et al. 2013, p. 200
19 Cowan et al. 2009, p. 586
20 Cowan et al. 2009, p. 586; Jan et al. 2009; Cowan et al. 2001, p. 187
21 Witvrouw et al. 2000, p. 484; Ophey et al. 2021, p. 301; Piva et al. 2005
22 Boling et al. 2009, p. 2110; McPoil et al. 2011, p. 293; Davis, Powers 2010, pp. A29
23 Callaghan, Baltzopoulos 1994, p. 84
24 Dierks et al. 2006; Lee et al. 1994; Tennant et al. 2001, p. 157; Souza, Powers 2009, p. 584; Davis, Powers 2010, pp. A27
25 Lee et al. 2003, p. 686; Salsich, Perman 2007, p. 521
26 Willson, Davis 2008a, p. 207
27 Willson, Davis 2008b, p. 606; Davis, Powers 2010, pp. A29; Noehren et al. 2013, p. 1122; Neal et al. 2016, p. 73; Rees et al. 2019, p. 227; Stefanyshyn et al. 2006, p. 1850
28 Cowan et al. 2009, p. 584; Willson, Davis 2009, p. 81; Souza, Powers 2009, p. 585; Neal et al. 2016, p. 73; Dierks et al. 2008, pp. 454–455
29 Baldon, Rodrigo de Marche et al. 2015, p. 1485; Zarei et al. 2020, p. 265; Earl-Boehm et al. 2018, p. 546; Dierks et al. 2011, p. 698; Foroughi et al. 2019, p. 221
30 Willson, Davis 2009, p. 76
31 Rezvanifar et al. 2019, p. 1235; Keser et al. 2008
32 Souza, Powers 2009, p. 580
33 Stefanyshyn et al. 2006, p. 1844
34 Dierks et al. 2011, p. 698
35 Boling et al. 2010, p. 728
36 Näslund et al. 2007, p. 1668; Selfe et al. 2003, p. 140; Sanchis-Alfonso et al. 2005
37 Baker et al. 2002, p. 213
38 Sutlive et al. 2004, p. 56
39 Prins, van der Wurff, Peter 2009, p. 14; Saad et al. 2018, p. 413; Rathleff et al. 2013, p. 5; Stefanyshyn et al. 2006, p. 1844
40 Csintalan et al. 2002; Lee et al. 2003, p. 688; Draper et al. 2009, p. 574; Neal et al. 2016, p. 75; Prins, van der Wurff, Peter 2009, p. 13
41 Selfe et al. 2016, p. 873; Selfe et al. 2018, p. 37
42 Sutlive et al. 2004, p. 50
43 Witvrouw et al. 2000, p. 485
44 Selhorst et al. 2020, p. 24; Selhorst et al. 2021, p. 1268
45 Selhorst et al. 2020, p. 24
46 Ferber et al. 2015, p. 373
47 Bolgla, Malone 2005, p. 80
48 Crossley et al. 2016, p. 848
49 Rabelo, Nayra Deise dos Anjos et al. 2017, p. 280
50 Steinberg et al. 2012, p. 563
51 Fernandez Cuadros, Marcos Edgar et al. 2017, p. 204
52 Crossley et al. 2016, p. 850
53 Vegstein et al. 2019, p. 923
54 Bizzini et al. 2003, p. 14; Jensen et al. 1999, pp. 523–525; Ma et al. 2020, p. 1682
55 Noehren et al. 2011, p. 694; Willy et al. 2012, p. 1049; Neal et al. 2016, p. 78; Davis et al. 2020, p. 105; Bonacci et al. 2018, p. 459
56 Bonacci et al. 2018, p. 460
Bibliography
Baker, Vanessa; Bennell, Kim; Stillman, Barry; Cowan, Sallie; Crossley, Kay (2002): Abnormal knee joint position sense in individuals with patellofemoral pain syndrome. In J. Orthop. Res. 20 (2), pp. 208–214. DOI: 10.1016/S0736-0266(01)00106-1.
Baldon, Rodrigo de Marche; Piva, Sara Regina; Scattone Silva, Rodrigo; Serrão, Fábio Viadanna (2015): Evaluating Eccentric Hip Torque and Trunk Endurance as Mediators of Changes in Lower Limb and Trunk Kinematics in Response to Functional Stabilization Training in Women With Patellofemoral Pain. In Am J Sports Med 43 (6), pp. 1485–1493. DOI: 10.1177/0363546515574690.
Barton, Christian J.; Webster, Kate E.; Menz, Hylton B. (2008): Evaluation of the Scope and Quality of Systematic Reviews on Nonpharmacological Conservative Treatment for Patellofemoral Pain Syndrome. In J Orthop Sports Phys Ther 38 (9), pp. 529–541. DOI: 10.2519/jospt.2008.2861.
Bizzini, Mario; Childs, John D.; Piva, Sara R.; Delitto, Anthony (2003): Systematic Review of the Quality of Randomized Controlled Trials for Patellofemoral Pain Syndrome. In J Orthop Sports Phys Ther 33 (1), pp. 4–20. DOI: 10.2519/jospt.2003.33.1.4.
Bolgla, Lori; Malone, Terry (2005): Exercise Prescription and Patellofemoral Pain: Evidence for Rehabilitation. In Journal of Sport Rehabilitation 14 (1), pp. 72–88. DOI: 10.1123/jsr.14.1.72.
Bolgla, Lori A.; Malone, Terry R.; Umberger, Brian R.; Uhl, Timothy L. (2008): Hip Strength and Hip and Knee Kinematics During Stair Descent in Females With and Without Patellofemoral Pain Syndrome. In J Orthop Sports Phys Ther 38 (1), pp. 12–18. DOI: 10.2519/jospt.2008.2462.
Boling, M.; Padua, D.; Marshall, S.; Guskiewicz, K.; Pyne, S.; Beutler, A. (2010): Gender differences in the incidence and prevalence of patellofemoral pain syndrome. In Scandinavian Journal of Medicine & Science in Sports 20 (5), pp. 725–730. DOI: 10.1111/j.1600-0838.2009.00996.x.
Boling, Michelle C.; Padua, Darin A.; Marshall, Stephen W.; Guskiewicz, Kevin; Pyne, Scott; Beutler, Anthony (2009): A Prospective Investigation of Biomechanical Risk Factors for Patellofemoral Pain Syndrome. In Am J Sports Med 37 (11), pp. 2108–2116. DOI: 10.1177/0363546509337934.
Bonacci, Jason; Hall, Michelle; Saunders, Natalie; Vicenzino, Bill (2018): Gait retraining versus foot orthoses for patellofemoral pain: a pilot randomised clinical trial. In Journal of Science and Medicine in Sport 21 (5), pp. 457–461. DOI: 10.1016/j.jsams.2017.09.187.
Callaghan, M. J.; Baltzopoulos, V. (1994): Gait analysis in patients with anterior knee pain. In Clinical Biomechanics 9 (2), pp. 79–84. DOI: 10.1016/0268-0033(94)90028-0.
Callaghan, Michael J.; Oldham, Jacqueline A. (2004): Electric muscle stimulation of the quadriceps in the treatment of patellofemoral pain11A commercial party with a direct financial interest in the results of the research supporting this article has conferred or will confer a financial benefit on the author or 1 or more of the authors. In Archives of Physical Medicine and Rehabilitation 85 (6), pp. 956–962. DOI: 10.1016/j.apmr.2003.07.021.
Collins, N.; Crossley, K.; Beller, E.; Darnell, R.; McPoil, T.; Vicenzino, B. (2009): Foot orthoses and physiotherapy in the treatment of patellofemoral pain syndrome: randomised clinical trial. In British Journal of Sports Medicine 43 (3), pp. 163–168. DOI: 10.1136/bmj.a1735.
Cook, Chad; Hegedus, Eric; Hawkins, Richard; Scovell, Field; Wyland, Doug (2010): Diagnostic Accuracy and Association to Disability of Clinical Test Findings Associated with Patellofemoral Pain Syndrome. In Physiotherapy Canada 62 (1), pp. 17–24. DOI: 10.3138/physio.62.1.17.
Cowan, S. M.; Crossley, K. M.; Bennell, K. L. (2009): Altered hip and trunk muscle function in individuals with patellofemoral pain. In British Journal of Sports Medicine 43 (8), pp. 584–588. DOI: 10.1136/bjsm.2008.053553.
Cowan, Sallie M.; Bennell, Kim L.; Hodges, Paul W.; Crossley, Kay M.; McConnell, Jenny (2001): Delayed onset of electromyographic activity of vastus medialis obliquus relative to vastus lateralis in subjects with patellofemoral pain syndrome. In Archives of Physical Medicine and Rehabilitation 82 (2), pp. 183–189. DOI: 10.1053/apmr.2001.19022.
Crossley, Kay M.; van Middelkoop, Marienke; Callaghan, Michael J.; Collins, Natalie J.; Rathleff, Michael Skovdal; Barton, Christian J. (2016): 2016 Patellofemoral pain consensus statement from the 4th International Patellofemoral Pain Research Retreat, Manchester. Part 2: recommended physical interventions (exercise, taping, bracing, foot orthoses and combined interventions). In Br J Sports Med 50 (14), pp. 844–852. DOI: 10.1136/bjsports-2016-096268.
Csintalan, Rick P.; Schulz, Michele M.; Woo, Jonathan; McMahon, Patrick J.; Lee, Thay Q. (2002): Gender Differences in Patellofemoral Joint Biomechanics. In Clinical Orthopaedics and Related Research 402, pp. 260–269. DOI: 10.1097/00003086-200209000-00026.
Davis, Irene S.; Powers, Christopher (2010): Patellofemoral Pain Syndrome: Proximal, Distal, and Local Factors—International Research Retreat, April 30–May 2, 2009, Baltimore, Maryland. In J Orthop Sports Phys Ther 40 (3), pp. A1. DOI: 10.2519/jospt.2010.0302.
Davis, Irene S.; Tenforde, Adam S.; Neal, Bradley S.; Roper, Jenevieve L.; Willy, Richard W. (2020): Gait Retraining as an Intervention for Patellofemoral Pain. In Curr Rev Musculoskelet Med 13 (1), pp. 103–114. DOI: 10.1007/s12178-020-09605-3.
Dierks, Tracy A.; Davis, Irene; Hamill, Joseph (2006): Lower Extremity Joint Timing During Prolonged Treadmill Running in Runners with Patellofemoral Joint Pain. In Medicine & Science in Sports & Exercise 38 (Supplement), pp. S121. DOI: 10.1249/00005768-200605001-01436.
Dierks, Tracy A.; Manal, Kurt T.; Hamill, Joseph; Davis, Irene (2011): Lower Extremity Kinematics in Runners with Patellofemoral Pain during a Prolonged Run. In Medicine & Science in Sports & Exercise 43 (4), pp. 693–700. DOI: 10.1249/MSS.0b013e3181f744f5.
Dierks, Tracy A.; Manal, Kurt T.; Hamill, Joseph; Davis, Irene S. (2008): Proximal and Distal Influences on Hip and Knee Kinematics in Runners With Patellofemoral Pain During a Prolonged Run. In J Orthop Sports Phys Ther 38 (8), pp. 448–456. DOI: 10.2519/jospt.2008.2490.
Draper, Christine E.; Besier, Thor F.; Santos, Juan M.; Jennings, Fabio; Fredericson, Michael; Gold, Garry E. et al. (2009): Using real-time MRI to quantify altered joint kinematics in subjects with patellofemoral pain and to evaluate the effects of a patellar brace or sleeve on joint motion. In J. Orthop. Res. 27 (5), pp. 571–577. DOI: 10.1002/jor.20790.
DUFFEY, MICHAEL J.; MARTIN, DAVID F.; CANNON, D. WAYNE; CRAVEN, TIMOTHY; MESSIER, STEPHEN P. (2000): Etiologic factors associated with anterior knee pain in distance runners. In Medicine & Science in Sports & Exercise 32 (11), pp. 1825–1832. DOI: 10.1097/00005768-200011000-00003.
Earl, Jennifer E.; Hoch, Anne Z. (2011): A Proximal Strengthening Program Improves Pain, Function, and Biomechanics in Women With Patellofemoral Pain Syndrome. In Am J Sports Med 39 (1), pp. 154–163. DOI: 10.1177/0363546510379967.
Earl-Boehm, Jennifer E.; Bolgla, Lori A.; Emory, Carolyn; Hamstra-Wright, Karrie L.; Tarima, Sergey; Ferber, Reed (2018): Treatment Success of Hip and Core or Knee Strengthening for Patellofemoral Pain: Development of Clinical Prediction Rules. In Journal of athletic training 53 (6), pp. 545–552. DOI: 10.4085/1062-6050-510-16.
Ferber, Reed; Bolgla, Lori; Earl-Boehm, Jennifer E.; Emery, Carolyn; Hamstra-Wright, Karrie (2015): Strengthening of the Hip and Core Versus Knee Muscles for the Treatment of Patellofemoral Pain: A Multicenter Randomized Controlled Trial. In Journal of athletic training 50 (4), pp. 366–377. DOI: 10.4085/1062-6050-49.3.70.
Ferber, Reed; Kendall, Karen D.; Farr, Lindsay (2011): Changes in Knee Biomechanics After a Hip-Abductor Strengthening Protocol for Runners With Patellofemoral Pain Syndrome. In Journal of athletic training 46 (2), pp. 142–149. DOI: 10.4085/1062-6050-46.2.142.
Fernandez Cuadros, Marcos Edgar; Albaladejo Florin, Maria Jesus; Lopez, Ruben Algarra; Perez Moro, Olga Susana (2017): Efficiency of Platelet-rich Plasma (PRP) Compared to Ozone Infiltrations on Patellofemoral Pain Syndrome and Chondromalacia: A Non- Randomized Parallel Controlled Trial. In Divers Equal Health Care 14 (4). DOI: 10.21767/2049-5471.1000112.
Foroughi, Forouzan; Sobhani, Sobhan; Yoosefinejad, Amin Kordi; Motealleh, Alireza (2019): Added Value of Isolated Core Postural Control Training on Knee Pain and Function in Women With Patellofemoral Pain Syndrome: A Randomized Controlled Trial. In Archives of Physical Medicine and Rehabilitation 100 (2), pp. 220–229. DOI: 10.1016/j.apmr.2018.08.180.
Fukuda, Thiago Yukio; Melo, William Pagotti; Zaffalon, Bruno Marcos; Rossetto, Flavio Marcondes; Magalhães, Eduardo; Bryk, Flavio Fernandes; Martin, Robroy L. (2012): Hip Posterolateral Musculature Strengthening in Sedentary Women With Patellofemoral Pain Syndrome: A Randomized Controlled Clinical Trial With 1-Year Follow-up. In J Orthop Sports Phys Ther 42 (10), pp. 823–830. DOI: 10.2519/jospt.2012.4184.
Haim, Amir; Yaniv, Moshe; Dekel, Samuel; Amir, Hagay (2006): Patellofemoral Pain Syndrome. In Clinical Orthopaedics and Related Research 451, pp. 223–228. DOI: 10.1097/01.blo.0000229284.45485.6c.
IRELAND, MARY LLOYD; Willson, John D.; BALLANTYNE, BRYON T.; DAVIS, IRENE MCCLAY (2003): Hip Strength in Females With and Without Patellofemoral Pain. In J Orthop Sports Phys Ther 33 (11), pp. 671–676. DOI: 10.2519/jospt.2003.33.11.671.
Jan, Mei-Hwa; Lin, Da-Hon; Lin, Jiu-Jenq; Lin, Chien-Ho Janice; Cheng, Cheng-Kung; Lin, Yeong-Fwu (2009): Differences in Sonographic Characteristics of the Vastus Medialis Obliquus between Patients with Patellofemoral Pain Syndrome and Healthy Adults. In Am J Sports Med 37 (9), pp. 1743–1749. DOI: 10.1177/0363546509333483.
Jensen, Roar; Gøthesen, Øystein; Liseth, Knut; Baerheim, Anders (1999): Acupuncture Treatment of Patellofemoral Pain Syndrome. In The Journal of Alternative and Complementary Medicine 5 (6), pp. 521–527. DOI: 10.1089/acm.1999.5.521.
Keser, Selçuk; Savranlar, Ahmet; Bayar, Ahmet; Ege, Ahmet; Turhan, Egemen (2008): Is there a relationship between anterior knee pain and femoral trochlear dysplasia? Assessment of lateral trochlear inclination by magnetic resonance imaging. In Knee Surg Sports Traumatol Arthr 16 (10), pp. 911–915. DOI: 10.1007/s00167-008-0571-5.
Khayambashi, Khalil; Mohammadkhani, Zeynab; Ghaznavi, Kourosh; Lyle, Mark A.; Powers, Christopher M. (2012): The Effects of Isolated Hip Abductor and External Rotator Muscle Strengthening on Pain, Health Status, and Hip Strength in Females With Patellofemoral Pain: A Randomized Controlled Trial. In J Orthop Sports Phys Ther 42 (1), pp. 22–29. DOI: 10.2519/jospt.2012.3704.
Lankhorst, Nienke E.; Bierma-Zeinstra, Sita M A; van Middelkoop, Marienke (2013): Factors associated with patellofemoral pain syndrome: a systematic review. In Br J Sports Med 47 (4), pp. 193–206. DOI: 10.1136/bjsports-2011-090369.
Lee, T. Q.; Anzel, S. H.; Bennett, K. A.; Pang, D.; Kim, W. C. (1994): The influence of fixed rotational deformities of the femur on the patellofemoral contact pressures in human cadaver knees. In Clinical Orthopaedics and Related Research (302), pp. 69–74.
Lee, Thay Q.; Morris, Garrett; Csintalan, Rick P. (2003): The Influence of Tibial and Femoral Rotation on Patellofemoral Contact Area and Pressure. In J Orthop Sports Phys Ther 33 (11), pp. 686–693. DOI: 10.2519/jospt.2003.33.11.686.
Leibbrandt, Dominique C.; Louw, Quinette A. (2018): Targeted Functional Movement Retraining to Improve Pain, Function, and Biomechanics in Subjects With Anterior Knee Pain: A Case Series. In Journal of Sport Rehabilitation 27 (3), pp. 218–223. DOI: 10.1123/jsr.2016-0164.
Levinger, Pazit; Gilleard, Wendy (2005): The heel strike transient during walking in subjects with patellofemoral pain syndrome. In Physical Therapy in Sport 6 (2), pp. 83–88. DOI: 10.1016/j.ptsp.2005.02.005.
Ma, Yan-Tao; Li, Li-Hui; Han, Qi; Wang, Xiao-Lei; Jia, Pei-Yu; Huang, Qiang-Min; Zheng, Yong-Jun (2020): Effects of Trigger Point Dry Needling on Neuromuscular Performance and Pain of Individuals Affected by Patellofemoral Pain: A Randomized Controlled Trial. In JPR Volume 13, pp. 1677–1686. DOI: 10.2147/JPR.S240376.
Magalhães, Eduardo; Fukuda, Thiago Yukio; Sacramento, Sylvio Noronha; Forgas, Andrea; Cohen, Moisés; Abdalla, Rene Jorge (2010): A Comparison of Hip Strength Between Sedentary Females With and Without Patellofemoral Pain Syndrome. In J Orthop Sports Phys Ther 40 (10), pp. 641–647. DOI: 10.2519/jospt.2010.3120.
Matthews, Mark; Rathleff, Michael Skovdal; Claus, Andrew; McPoil, Tom; Nee, Robert; Crossley, Kay M. et al. (2020): Does foot mobility affect the outcome in the management of patellofemoral pain with foot orthoses versus hip exercises? A randomised clinical trial. In Br J Sports Med 54 (23), pp. 1416–1422. DOI: 10.1136/bjsports-2019-100935.
McPoil, Thomas G.; Warren, Meghan; Vicenzino, Bill; Cornwall, Mark W. (2011): Variations in Foot Posture and Mobility Between Individuals with Patellofemoral Pain and Those in a Control Group. In Journal of the American Podiatric Medical Association 101 (4), pp. 289–296. DOI: 10.7547/1010289.
Nakagawa, Theresa Helissa; Muniz, Thiago Batista; Baldon, Rodrigo de Marche; Dias Maciel, Carlos; de Menezes Reiff, Rodrigo Bezerra; Serrão, Fábio Viadanna (2008): The effect of additional strengthening of hip abductor and lateral rotator muscles in patellofemoral pain syndrome: a randomized controlled pilot study. In Clin Rehabil 22 (12), pp. 1051–1060. DOI: 10.1177/0269215508095357.
Näslund, Jan; Walden, Markus; Lindberg, Lars-Göran (2007): Decreased Pulsatile Blood Flow in the Patella in Patellofemoral Pain Syndrome. In Am J Sports Med 35 (10), pp. 1668–1673. DOI: 10.1177/0363546507303115.
Neal, Bradley S.; Barton, Christian J.; Gallie, Rosa; O’Halloran, Patrick; Morrissey, Dylan (2016): Runners with patellofemoral pain have altered biomechanics which targeted interventions can modify: A systematic review and meta-analysis. In Gait & Posture 45, pp. 69–82. DOI: 10.1016/j.gaitpost.2015.11.018.
Neal, Bradley S.; Lack, Simon D.; Lankhorst, Nienke E.; Raye, Andrew; Morrissey, Dylan; van Middelkoop, Marienke (2019): Risk factors for patellofemoral pain: a systematic review and meta-analysis. In Br J Sports Med 53 (5), pp. 270–281. DOI: 10.1136/bjsports-2017-098890.
Noehren, B.; Scholz, J.; Davis, I. (2011): The effect of real-time gait retraining on hip kinematics, pain and function in subjects with patellofemoral pain syndrome. In British Journal of Sports Medicine 45 (9), pp. 691–696. DOI: 10.1136/bjsm.2009.069112.
Noehren, Brian; Hamill, Joseph; Davis, Irene (2013): Prospective Evidence for a Hip Etiology in Patellofemoral Pain. In Medicine & Science in Sports & Exercise 45 (6), pp. 1120–1124. DOI: 10.1249/MSS.0b013e31828249d2.
Nunes, Guilherme S.; Wolf, Débora Faria; dos Santos, Daniel Augusto; Noronha, Marcos de; Serrão, Fábio Viadanna (2020): Acute Effects of Hip Mobilization With Movement Technique on Pain and Biomechanics in Females With Patellofemoral Pain: A Randomized, Placebo-Controlled Trial. In Journal of Sport Rehabilitation 29 (6), pp. 707–715. DOI: 10.1123/jsr.2018-0497.
Ophey, Martin J.; Crooijmans, Gwen A.H.M.; Frieling, Sophie M.W.; Kardos, Donja M.A.; van den Berg, Robert; Kerkhoffs, Gino M.M.J.; Tak, Igor J.R. (2021): Short-term effectiveness of an intervention targeting lower limb range of motion on pain and disability in patellofemoral pain patients: A randomized, non-concurrent multiple-baseline study. In Journal of Bodywork and Movement Therapies 26 (18), pp. 300–308. DOI: 10.1016/j.jbmt.2020.12.028.
Piva, Sara R.; Goodnite, Edward A.; Childs, John D. (2005): Strength Around the Hip and Flexibility of Soft Tissues in Individuals With and Without Patellofemoral Pain Syndrome. In J Orthop Sports Phys Ther 35 (12), pp. 793–801. DOI: 10.2519/jospt.2005.35.12.793.
Prins, Maarten R.; van der Wurff, Peter (2009): Females with patellofemoral pain syndrome have weak hip muscles: a systematic review. In Australian Journal of Physiotherapy 55 (1), pp. 9–15. DOI: 10.1016/s0004-9514(09)70055-8.
Priore, Liliam B.; Lack, Simon; Garcia, Carmen; Azevedo, Fabio M.; de Oliveira Silva, Danilo (2020): Two Weeks of Wearing a Knee Brace Compared With Minimal Intervention on Kinesiophobia at 2 and 6 Weeks in People With Patellofemoral Pain: A Randomized Controlled Trial. In Archives of Physical Medicine and Rehabilitation 101 (4), pp. 613–623. DOI: 10.1016/j.apmr.2019.10.190.
Rabelo, Nayra Deise dos Anjos; Costa, Leonardo Oliveira Pena; Lima, Bruna Maria de; dos Reis, Amir Curcio; Bley, André Serra; Fukuda, Thiago Yukio; Lucareli, Paulo Roberto Garcia (2017): Adding motor control training to muscle strengthening did not substantially improve the effects on clinical or kinematic outcomes in women with patellofemoral pain: A randomised controlled trial. In Gait & Posture 58 (4), pp. 280–286. DOI: 10.1016/j.gaitpost.2017.08.018.
Rathleff, Camilla Rams; Baird, William Neill; Olesen, Jens Lykkegaard; Roos, Ewa Maria; Rasmussen, Sten; Rathleff, Michael Skovdal; Hug, François (2013): Hip and Knee Strength Is Not Affected in 12-16 Year Old Adolescents with Patellofemoral Pain – A Cross-Sectional Population-Based Study. In PLoS ONE 8 (11), pp. e79153. DOI: 10.1371/journal.pone.0079153.
Rees, David; Younis, Ahmed; MacRae, Siân (2019): Is there a correlation in frontal plane knee kinematics between running and performing a single leg squat in runners with patellofemoral pain syndrome and asymptomatic runners? In Clinical Biomechanics 61 (7), pp. 227–232. DOI: 10.1016/j.clinbiomech.2018.12.008.
Rezvanifar, S. Cyrus; Flesher, Brett L.; Jones, Kerwyn C.; Elias, John J. (2019): Lateral patellar maltracking due to trochlear dysplasia: A computational study. In The Knee 26 (6), pp. 1234–1242. DOI: 10.1016/j.knee.2019.11.006.
Robinson, Ryan L.; Nee, Robert J. (2007): Analysis of Hip Strength in Females Seeking Physical Therapy Treatment for Unilateral Patellofemoral Pain Syndrome. In J Orthop Sports Phys Ther 37 (5), pp. 232–238. DOI: 10.2519/jospt.2007.2439.
Saad, Marcelo Camargo; Vasconcelos, Rodrigo Antunes de; Mancinelli, Letícia Villani de Oliveira; Munno, Matheus Soares de Barros; Liporaci, Rogério Ferreira; Grossi, Débora Bevilaqua (2018): Is hip strengthening the best treatment option for females with patellofemoral pain? A randomized controlled trial of three different types of exercises. In Brazilian Journal of Physical Therapy 22 (5), pp. 408–416. DOI: 10.1016/j.bjpt.2018.03.009.
Salsich, Gretchen B.; Perman, William H. (2007): Patellofemoral Joint Contact Area Is Influenced by Tibiofemoral Rotation Alignment in Individuals Who Have Patellofemoral Pain. In J Orthop Sports Phys Ther 37 (9), pp. 521–528. DOI: 10.2519/jospt.2007.37.9.521.
Saltychev, M.; Dutton, R.; Laimi, K.; Beaupré, G.; Virolainen, P.; Fredericson, M. (2018): Effectiveness of conservative treatment for patellofemoral pain syndrome: A systematic review and meta-analysis. In J Rehabil Med 50 (5), pp. 393–401. DOI: 10.2340/16501977-2295.
Sanchis-Alfonso, Vicente; Roselló-Sastre, Esther; Revert, Fernando; García, Almudena (2005): Histologic Retinacular Changes Associated With Ischemia in Painful Patellofemoral Malalignment. In Orthopedics 28 (6), pp. 593–599. DOI: 10.3928/0147-7447-20050601-16.
Selfe, J.; Harper, L.; Pedersen, I.; Breen-Turner, J.; Waring, J.; Stevens, D. (2003): Cold legs: a potential indicator of negative outcome in the rehabilitation of patients with patellofemoral pain syndrome. In The Knee 10 (2), pp. 139–143. DOI: 10.1016/S0968-0160(02)00085-6.
Selfe, James; Janssen, Jessie; Callaghan, Michael; Witvrouw, Erik; Sutton, Chris; Richards, Jim et al. (2016): Are there three main subgroups within the patellofemoral pain population? A detailed characterisation study of 127 patients to help develop targeted intervention (TIPPs). In Br J Sports Med 50 (14), pp. 873–880. DOI: 10.1136/bjsports-2015-094792.
Selfe, James; Janssen, Jessie; Drew, Benjamin; Dey, Paola (2018): Anterior knee pain subgroups: the first step towards a personalized treatment. In Ann. Joint 3, p. 32. DOI: 10.21037/aoj.2018.03.16.
Selhorst, Mitchell; Fernandez-Fernandez, Alicia; Schmitt, Laura; Hoehn, Jessica (2021): Effect of a Psychologically Informed Intervention to Treat Adolescents With Patellofemoral Pain: A Randomized Controlled Trial. In Archives of Physical Medicine and Rehabilitation 102 (7), pp. 1267–1273. DOI: 10.1016/j.apmr.2021.03.016.
Selhorst, Mitchell; Hoehn, Jessica; Degenhart, Todd; Schmitt, Laura; Fernandez-Fernandez, Alicia (2020): Psychologically-informed video reduces maladaptive beliefs in adolescents with patellofemoral pain. In Physical Therapy in Sport 41 (2018), pp. 23–28. DOI: 10.1016/j.ptsp.2019.10.009.
Song, Chen-Yi; Lin, Yeong-Fwu; Wei, Tung-Ching; Lin, Da-Hon; Yen, Tzu-Yu; Jan, Mei-Hwa (2009): Surplus Value of Hip Adduction in Leg-Press Exercise in Patients With Patellofemoral Pain Syndrome: A Randomized Controlled Trial. In Physical Therapy 89 (5), pp. 409–418. DOI: 10.2522/ptj.20080195.
Souza, Richard B.; Powers, Christopher M. (2009): Predictors of Hip Internal Rotation during Running. In Am J Sports Med 37 (3), pp. 579–587. DOI: 10.1177/0363546508326711.
Stefanyshyn, Darren J.; Stergiou, Pro; Lun, Victor M. Y.; Meeuwisse, Willem H.; Worobets, Jay T. (2006): Knee Angular Impulse as a Predictor of Patellofemoral Pain in Runners. In Am J Sports Med 34 (11), pp. 1844–1851. DOI: 10.1177/0363546506288753.
Steinberg, N.; Siev-Ner, I.; Peleg, S.; Dar, G.; Masharawi, Y.; Zeev, A.; Hershkovitz, I. (2012): Joint Range of Motion and Patellofemoral Pain in Dancers. In Int J Sports Med 33 (07), pp. 561–566. DOI: 10.1055/s-0031-1301330.
Sutlive, Thomas G.; Mitchell, Scott D.; Maxfield, Stephanie N.; McLean, Cynthia L.; Neumann, Jon C.; Swiecki, Christine R. et al. (2004): Identification of Individuals With Patellofemoral Pain Whose Symptoms Improved After a Combined Program of Foot Orthosis Use and Modified Activity: A Preliminary Investigation. In Physical Therapy 84 (1), pp. 49–61. DOI: 10.1093/ptj/84.1.49.
Tennant, S.; Williams, A.; Vedi, V.; Kinmont, C.; Gedroyc, W.; Hunt, D. (2001): Patello-femoral tracking in the weight-bearing knee: a study of asymptomatic volunteers utilising dynamic magnetic resonance imaging: a preliminary report. In Knee Surg Sports Traumatol Art 9 (3), pp. 155–162. DOI: 10.1007/s001670000173.
van Cant, Joachim; Pitance, Laurent; Feipel, Véronique (2017): Hip abductor, trunk extensor and ankle plantar flexor endurance in females with and without patellofemoral pain. In BMR 30 (2), pp. 299–307. DOI: 10.3233/BMR-150505.
van der Heijden, Rianne A; Lankhorst, Nienke E.; van Linschoten, Rabbart; Bierma-Zeinstra, Sita M.; van Middelkoop, Marienke (2016): Exercise for treating patellofemoral pain syndrome: an abridged version of Cochrane systematic review. In European journal of physical and rehabilitation medicine 52 (1), pp. 110–133.
van der Heijden, Rianne A; Lankhorst, Nienke E.; van Linschoten, Robbart; Bierma-Zeinstra, Sita M. A.; van Middelkoop, Marienke (2015): Exercise for treating patellofemoral pain syndrome. In Cochrane Database of Systematic Reviews 5 (1), pp. 1–204. DOI: 10.1002/14651858.CD010387.pub2.
van Linschoten, R.; van Middelkoop, M.; Berger, M. Y.; Heintjes, E. M.; Verhaar, J A N; Willemsen, S. P. et al. (2009): Supervised exercise therapy versus usual care for patellofemoral pain syndrome: an open label randomised controlled trial. In BMJ 339 (oct20 1), pp. b4074. DOI: 10.1136/bmj.b4074.
van Linschoten, Robbart; van Middelkoop, Marienke; Berger, Marjolein Y.; Heintjes, Edith M.; Koopmanschap, Mark A.; Verhaar, Jan A. N. et al. (2006): The PEX study – Exercise therapy for patellofemoral pain syndrome: design of a randomized clinical trial in general practice and sports medicine [ISRCTN83938749]. In BMC Musculoskelet Disord 7 (1), p. 207. DOI: 10.1186/1471-2474-7-31.
Vegstein, Kristine; Robinson, Hilde Stendal; Jensen, Roar (2019): Neurodynamic tests for patellofemoral pain syndrome: a pilot study. In Chiropr Man Therap 27 (1), p. 923. DOI: 10.1186/s12998-019-0242-2.
Willson, John D.; Davis, Irene S. (2008a): Lower extremity mechanics of females with and without patellofemoral pain across activities with progressively greater task demands. In Clinical Biomechanics 23 (2), pp. 203–211. DOI: 10.1016/j.clinbiomech.2007.08.025.
Willson, John D.; Davis, Irene S. (2008b): Utility of the Frontal Plane Projection Angle in Females With Patellofemoral Pain. In J Orthop Sports Phys Ther 38 (10), pp. 606–615. DOI: 10.2519/jospt.2008.2706.
Willson, John D.; Davis, Irene S. (2009): Lower Extremity Strength and Mechanics during Jumping in Women with Patellofemoral Pain. In Journal of Sport Rehabilitation 18 (1), pp. 76–90. DOI: 10.1123/jsr.18.1.76.
Willy, Richard W.; Scholz, John P.; Davis, Irene S. (2012): Mirror gait retraining for the treatment of patellofemoral pain in female runners. In Clinical Biomechanics 27 (10), pp. 1045–1051. DOI: 10.1016/j.clinbiomech.2012.07.011.
Witvrouw, Erik; Lysens, Roeland; Bellemans, Johan; Cambier, Dirk; Vanderstraeten, Guy (2000): Intrinsic Risk Factors for the Development of Anterior Knee Pain in an Athletic Population: A Two-Year Prospective Study. In Am J Sports Med 28 (4), pp. 480–489. DOI: 10.1177/03635465000280040701.
Yañez-Álvarez, Angel; Bermúdez-Pulgarín, Beatriz; Hernández-Sánchez, Sergio; Albornoz-Cabello, Manuel (2020): Effects of exercise combined with whole body vibration in patients with patellofemoral pain syndrome: a randomised-controlled clinical trial. In BMC Musculoskelet Disord 21 (1), p. 839. DOI: 10.1186/s12891-020-03599-2.
Zarei, Hanieh; Bervis, Soha; Piroozi, Soraya; Motealleh, Alireza (2020): Added Value of Gluteus Medius and Quadratus Lumborum Dry Needling in Improving Knee Pain and Function in Female Athletes With Patellofemoral Pain Syndrome: A Randomized Clinical Trial. In Archives of Physical Medicine and Rehabilitation 101 (2), pp. 265–274. DOI: 10.1016/j.apmr.2019.07.009.
